History Of Human Corona Virus
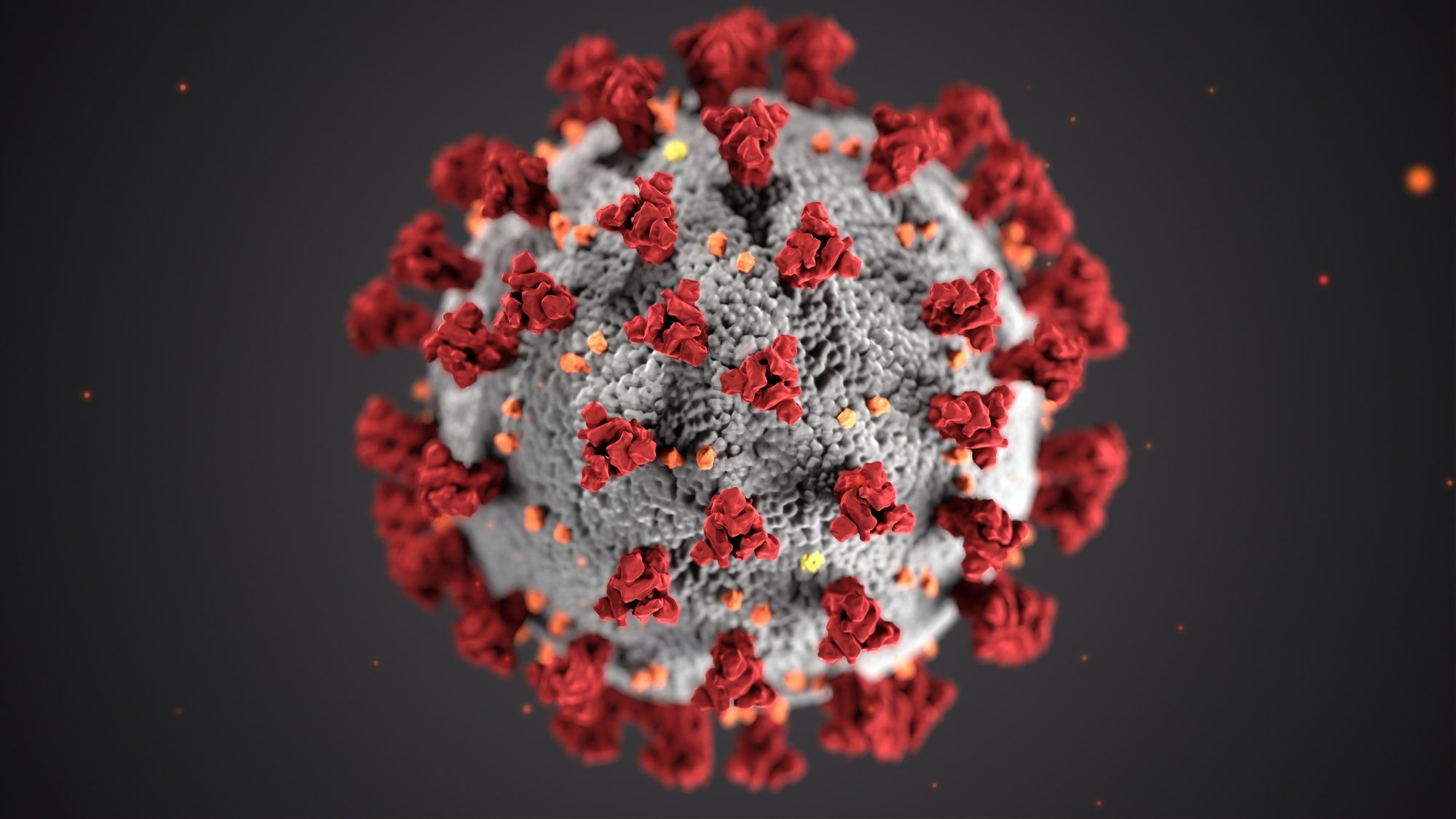
Corona virus aka COVID-19, SARS-CoV-2. coronavirus, any contagion belonging to the family Coronaviridae. Coronaviruses have enveloped virions (contagion patches) that measure roughly 120 nm (1 nm = 10 − 9 meter) in fringe. Club- shaped glycoprotein spikes within the envelope give the contagions a crownlike, or coronal, appearance. The nucleocapsid, made from a protein shell referred to as a capsid and containing the viral nucleic acids, is helical or tubular. The coronavirus genome consists of one beachfront of positive- sense RNA (ribonucleic acid). Coronaviridae is generally considered to contain two rubrics, Coronavirus and Torovirus, which differ in nucleocapsid morphology, the former being helical and therefore the ultimate being tubular. Coronaviruses are important agents of gastrointestinal complaint in humans, meat, and bovines. In humans, a species appertained to as SARS coronavirus (or Severe acute respiratory pattern coronavirus) causes a largely contagious respiratory disease that's characterized by symptoms of fever, cough, and muscle stitch, constantly with progressive difficulty in breathing. The contagion surfaced in humans in 2002;
it likely jumped to humans from an beast force, believed to be horseshoe bludgeons. The capability of SARS coronavirus to vault to humans really demanded heritable changes within the contagion. These changes are suspected to retain passed within the palm cat, since the SARS contagion present in horseshoe bludgeons is unfit to infect humans directly. In 2012 another coronavirus suitable of causing a severe acute respiratory complaint subsequently appertained to as Middle East respiratory pattern (MERS) was discovered in humans. The first case was factory in Saudi Arabia, and others were reported within the preceding time in France, Germany, Jordan, Qatar, Tunisia, the United Arab Emirates, and the United Kingdom. All vindicated cases were directly or indirectly linked to the center East. Of all vindicated cases proved by 2019, roughly one-third had led to death. The new MERS coronavirus was nearly like other coronaviruses known to retain began in bludgeons and was allowed to be passed from bludgeons to other brutes before being transmitted to humans. Camels were linked together possible force for the MERS contagion.
Where Did the Coronavirus Come From?
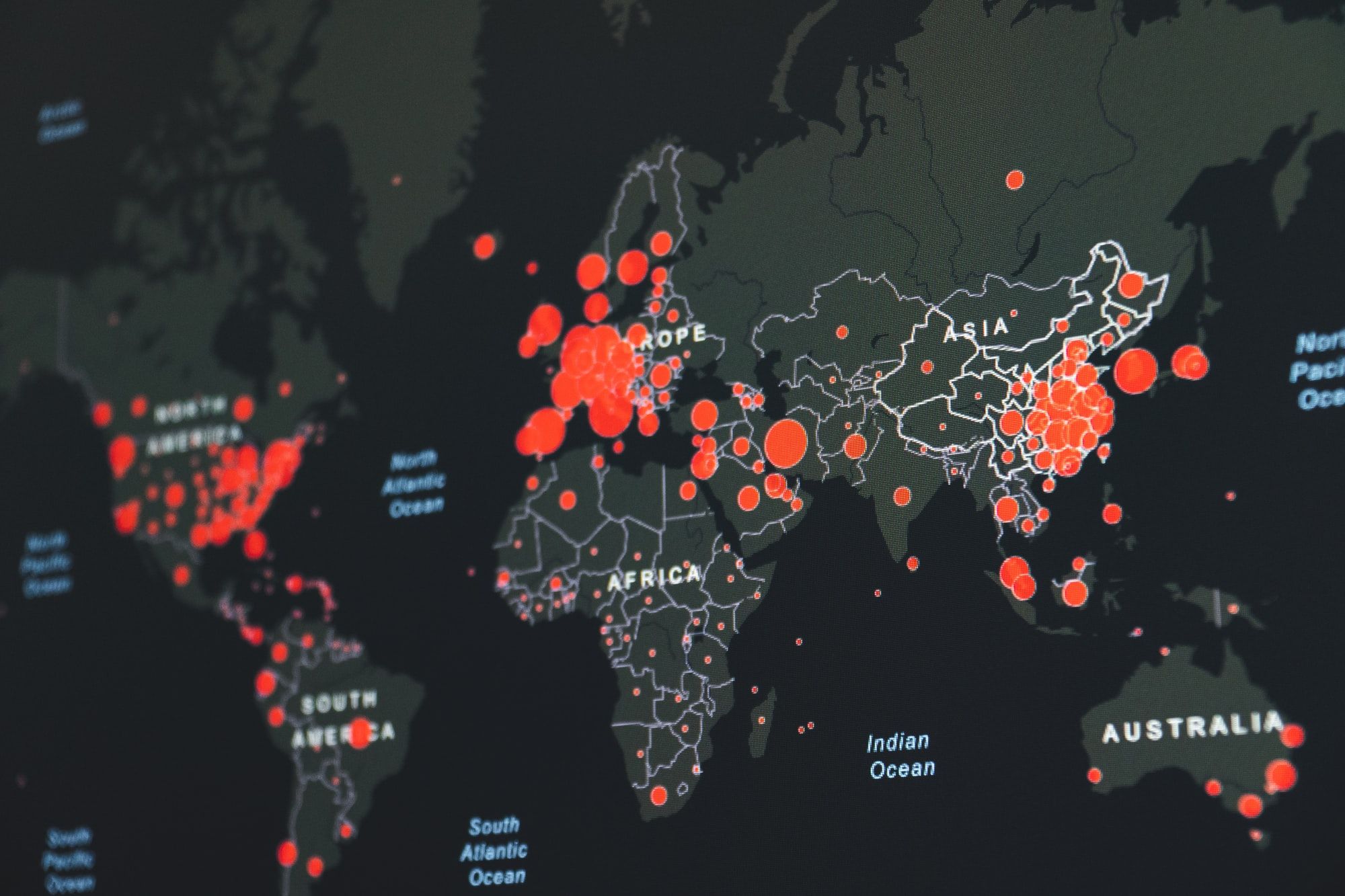
Experts say SARS-CoV-2 began in batons. That’s also how the coronaviruses behind Middle East respiratory pattern (MERS) and severe acute respiratory pattern (SARS) got started.SARS-CoV-2 made the jump to humans at one of Wuhan’s open- air “ wet requests.” They ’re where guests buy fresh meat and fish, including creatures that are killed on the spot. Some wet requests vend wild or banned species like cobras, wild boars, and raccoon tykes. Crowded conditions can let contagions from different creatures exchange genes. Occasionally the contagion changes such a lot it can start to infect and spread among people. Still, the Wuhan request didn’t vend batons at the time of the outbreak. That’s why early dubitation also fell on pangolins, also called scaled anteaters, which are vended immorally in some requests in China. Some coronaviruses that infect pangolins are analogous to SARS-CoV-2.As SARS-CoV-2 spread both inside and out of doors China, it infected folks that have had no direct contact with creatures. That meant the contagion is transmitted from one mortal to a different . It’s now spreading in the U.S. and round the globe, meaning that folks are unwittingly catching and spending on the coronavirus.
This growing worldwide transmission is what's now a epidemic. On January 9 of this time, Chinese state media reported that a platoon of experimenters led by Xu Jianguo had linked the pathogen behind a mysterious outbreak of pneumonia in Wuhan as a new coronavirus. Although the contagion was soon after named 2019-nCoV, and also renamed SARS-CoV-2, it remains generally known simply because the coronavirus. While that moniker has been pelted into the stratosphere of public attention, it’s kindly deceiving Not only is it one of numerous coronaviruses out there, but you ’ve nearly clearly been infected with members of the family long before SARS-CoV-2’s emergence in late 2019.Coronaviruses take their name from the distinctive harpoons with rounded tips that embellish their face, which reminded virologists of the looks of the sun’s atmosphere, referred to as its nimbus. Colorful coronaviruses infect multitudinous species, but the primary mortal coronaviruses weren’t discovered until themid-1960s.“ That was sort of the golden days, if you will, of virology, because at that time the technology came available to grow contagions in the laboratory, and to study contagions in the laboratory,” says University of Texas Southwestern Medical Center pediatrician Jeffrey Kahn, who studies respiratory contagions. But the two coronaviruses that were linked at the time, OC43 and 229E, didn’t evoke important exploration interest, says Kahn, who wrote a review on coronaviruses a many times after the SARS outbreak of 2003. “ I don't believe there was an enormous trouble to form vaccines against these because these were allowed to be further of a nuisance than anything differently.”

The contagions beget typical cold symptoms similar as a sore throat, cough, and stuffy nose, and they sounded to be veritably common; one early study estimated that 3 percent of respiratory ails in a children’s home in Georgia over seven times in the 1960s had been caused by OC43, and a 1986 study of children and grown-ups in northern Italy plant that it was rare to come across a subject who didn't have antibodies to that contagion (an index of once infection).
Coronaviruses’ mild-mannered character changed with the SARS outbreak. Although related to OC43 and 229E, SARS-cov-2 was far deadlier, killing about 10 percent of people it infected — a aggregate of 774 worldwide, according to the United Kingdom’s National Health Service. While it’s still unclear exactly where SARS-cov-2 came from, analogous contagions were latterly plant in batons, and some studies suggested the contagion could have jumped to humans via an conciliator similar as civets.
See “ Where Coronaviruses Come From”
While SARS was a wake-up call that coronaviruses posed a lesser threat to humans than had been allowed, it’s unsurprising that a contagion that’s recently revealed over to humans would be more deadly than its mortal- acclimated relatives, says Rachel Roper, a virologist and immunologist at East Carolina University. “ When a species is co-evolving with its pathogen... they tend to come to a conflict, where the contagion will be surviving in the population, and the population is surviving without that important illness,” she explains. “ But when a contagion jumps species, also you ’ve got a real problem.”
In the wake of the SARS epidemic, some experimenters went looking for other mortal coronaviruses — and plant them. In 2004, experimenters in the Netherlands reported they ’d plant a new coronavirus, related to 229E, in a child with pneumonia and in four other people with respiratory complaint. That contagion came to be known as NL63, and Kahn and his associates plant it at around the same time in rehabilitated children in New Haven, Connecticut (Kahn worked at Yale University School of Medicine at the time).
Although first linked in people with severe infections, NL63 is, much like 229E and OC43, a wide contagion that causes snap in utmost people it infects. But there were hints that its goods could extend beyond the respiratory tract. In their 2005 paper on the recently- discovered contagion, Kahn and his associates reported chancing it in 8 of 11 cases they tested who had Kawasaki complaint, an inflammation of the blood vessels that occurs primarily in youthful children. But utmost follow-up studies failed to find such an association.
“ It could be that it was just chance,” Kahn says of his finding, or “ there may be a signal there.” His 15- time-old study has acquired new salience in light of reports that COVID-19 is associated with Kawasaki-suchlike symptoms in some children, but he cautions that this seditious pattern has been defined slightly else by different groups reporting on it, and isn’t identical to Kawasaki complaint.
Close on the heels of NL63’s discovery came a report from Hong Kong on yet another common, cold-causing coronavirus, this bone called HKU1. As with NL63, experimenters in other corridor of the world went looking for HKU1, chancing it in Australia, France, and the United States, among other places.
The cold-causing coronaviruses each carry a analogous array of symptoms, says Kahn, and it’s not clear how long any of them have been hosted by humans, or where they came from firstly. As ubiquitous as they are, other introductory questions about these contagions also remain open, similar as whether infection with one of them confers lasting impunity. Studies reported in two recent preprints plant that it’s not uncommon for a person to be infected with the same coronavirus doubly. But Roper suspects that our bodies do learn to forfend off coronaviruses they ’ve encountered. “ There are literally thousands of respiratory contagions, so presumably every time you get a deep freeze, you ’re getting a new contagion that you ’ve now days seen ahead,” she says. “ Plus, they ’re always shifting.”
Until the emergence of SARS-CoV-2, mortal coronaviruses that have made the news have been both far more deadly and far more contained than their cold-causing counterparts. No cases of SARS have been detected since 2004, and Middle East respiratory pattern coronavirus (MERS-CoV), first plant in a case in Saudi Arabia in 2012, has caused lower than vindicated cases worldwide, according to the World Health Organization — but it kills about 35 percent of people with vindicated judgments.
Variants of Coronavirus
How Do Variants Happen?
coronaviruses have all their inheritable material in commodity called RNA (ribonucleic acid). RNA has some parallels to DNA, but they are not the same.
When contagions infect you, they attach to your cells, get inside them, and make clones of their RNA, which helps them spread. However, the RNA gets changed, If there is a copying mistake. Scientists call those changes mutations.
These changes be aimlessly and by accident. It's a normal part of what happens to contagions as they multiply and spread.
Because the changes are arbitrary, they may make little to no difference in a person's health. Other times, they may beget complaint. For illustration, one reason you need a flu shot every time is because influenza contagions change from time to time. This time's flu contagion presumably is not the exact same bone that circulated last time.
Still, that variant will come more common, If a contagion has a arbitrary change that makes it easier to infect people and it spreads.
The nethermost line is that all contagions, including coronaviruses, can change over time.
Following are the variants / mutations of Sars-covid-2
- Alpha (B.1.1.7 and Q lineages)
- Beta (B.1.351 and descendent lineages)
- Gamma (P.1 and descendent lineages)
- Epsilon (B.1.427 and B.1.429)
- Eta (B.1.525)
- Iota (B.1.526)
- Kappa (B.1.617.1)
- 1.617.3
- Mu (B.1.621, B.1.621.1)
- Zeta (P.2)
- Delta (B.1.617.2 and AY lineages)
- Omicron (B.1.1.529 and BA lineages)
What Is the Omicron Variant?
The new variant (B.1.1.529) was first detected in samples collected on November 11, 2021 in Botswana. Experts in South Africa first reported the Omicron variant to the World Health Organization (WHO) on Nov. 24, 2021. They discovered the variant after COVID-19 infections suddenly began to go up.
The WHO grouped Omicron as a “ Variant of Concern.” This order means the variant might have a advanced transmissibility, beget more violent complaint, and may be less likely to respond to vaccines or treatments. But experimenters need further information to confirm these factors.
Early substantiation suggests that the Omicron variant causes a advanced threat of reinfection compared to other variants.
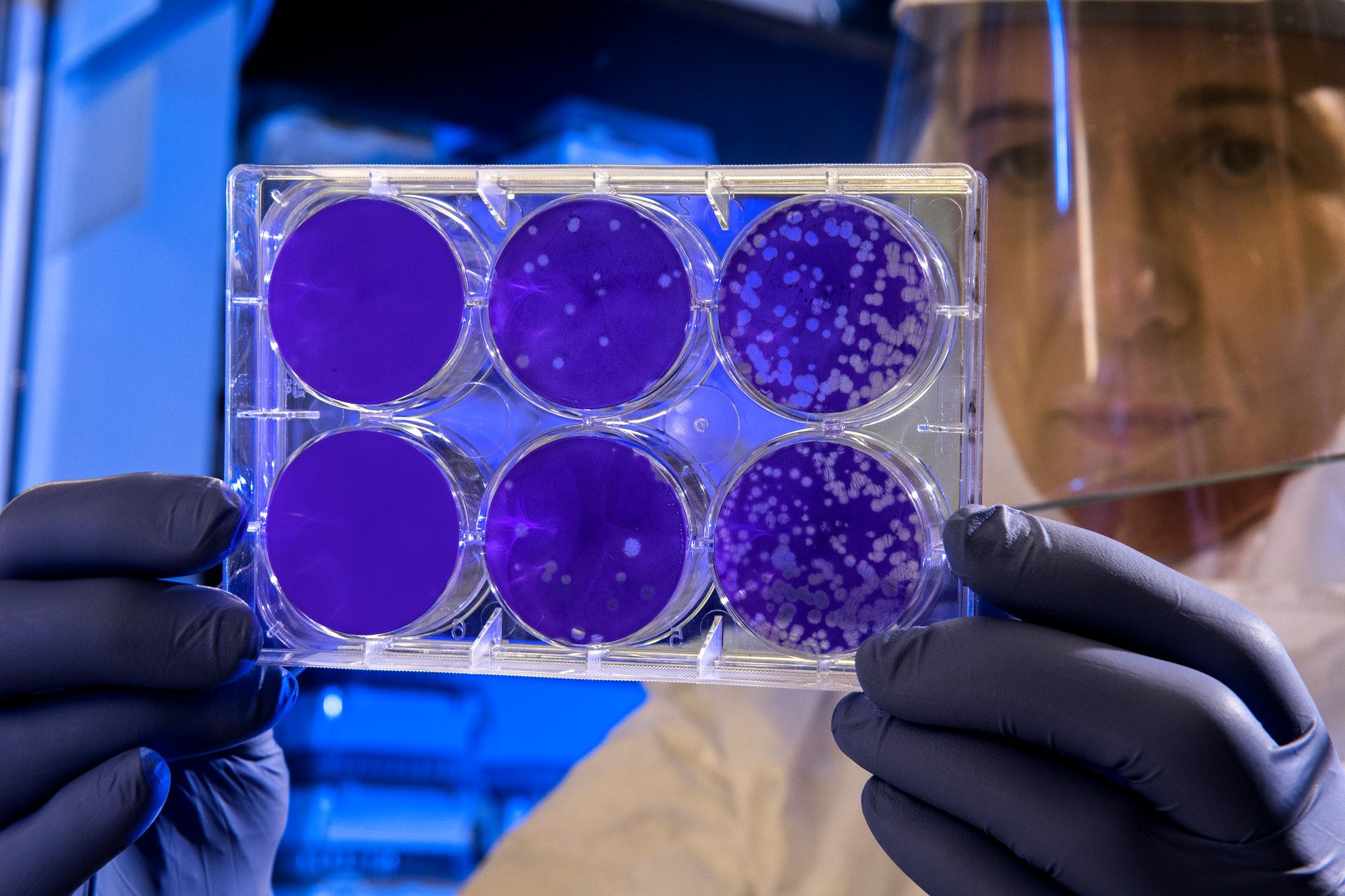
Current PCR tests for COVID-19 can effectively find Omicron cases. Experts plant that one specific PCR test does not identify one of the three target genes ( called the S gene powerhouse) in people infected with Omicron. Because of this, these tests can specifically mark positive Omicron cases and, because of that, can descry this variant briskly than with former surges.
According to exploration, advance infections are possible with the Omicron variant indeed if you ’re completely vaccinated. Still, COVID-19 vaccines and boosters are still effective at precluding severe illness, hospitalizations, and death.
The Omicron variant is now the dominant strain in the U.S.
Experts are keeping a close eye on how the variant spreads or develops.
In the meantime, experts recommend guarding yourself by getting the vaccine or a supporter if you ’re eligible for it. Wear a mask and maintain social distance. However, insulate yourself for 10 days, If you test positive for COVID or if you ’ve come in close contact with someone who has it. Call your croaker if you notice symptoms.
Other Coronavirus Mutations
Nascence(B.1.1.7). In late 2020, experts noted gene mutations in COVID-19 cases seen in people in southeastern England. This variant has ago been reported in other countries, including the U.S. Scientists estimate that these mutations could make the contagion up to 70 further transmittable, meaning it could spread more fluently. Some exploration has linked this variant to a advanced threat of death, but the substantiation is not strong.
The mutation on the Nascence variant is on the shaft protein, which helps the contagion infect its host. This is what COVID-19 vaccines target. These vaccines make antibodies against numerous corridor of the shaft protein, so it's doubtful that a single new mutation in the Nascence variant will make the vaccine less effective.
Beta (B.1.351). Other variants of the contagion have been plant in other countries, including South Africa and Nigeria. The Beta variant appears to spread more fluently than the original contagion but does not feel to beget worse illness.
Gamma (P. 1). In January 2021, experts spotted this COVID-19 variant in people from Brazil who'd traveled to Japan. By the end of that month, it was showing up in the U.S.
The Gamma variant appears to be more contagious than earlier strains of the contagion. And it may be suitable to infect people who've formerly had COVID-19. A report from Brazil confirms that a 29- time-old woman came down with this variant after an earlier coronavirus infection a many months ahead.
Some early exploration suggests that the variant's changes might help it shirk antibodies ( made by your vulnerable system after an infection or a vaccine) that fight the coronavirus. A lab study shows that the Pfizer-BioNTech vaccine can neutralize the fast- spreading Brazil strain. But more exploration is demanded.
Delta (B.1.617.2). This variant was spotted in India in December 2020. It caused a huge swell in cases in mid-April 2021. This largely contagious variant is now plant in 178 countries including the U.S., the U.K., Australia, and all of Europe. It's the dominant strain in the U.S. and the U.K.
A study of the COVID-19 vaccine's effectiveness against this variant plant that
Two boluses of the Pfizer-BioNTech vaccine were 88 effective 2 weeks after the alternate cure.
Two boluses of the AstraZeneca vaccine available in the U.K. were 60 effective.
Both vaccines are only 33 effective 3 weeks after the first cure.
Given the difference in protection between boluses, experts recommend getting the alternate shot as soon as you are eligible.
Research suggests that changes to the shaft protein may make the Delta variant up to 50 further transmittable than other COVID-19 variants.
For people who have not had the coronavirus vaccine, the Delta variant may beget more severe illness than the original strain of the contagion. Vaccinated people may also get what is called a “ advance infection,” but they are less likely to be seriously sick or to die. The fairly low rate of vaccination in some areas of the country is the main reason that the Delta variant has been suitable to spread so fleetly and shows no signs of decelerating down. Getting the vaccine is the stylish way to decelerate the spread of the coronavirus and cover yourself against serious illness or death.
Mu (B.1.621). Experts first spotted this COVID-19 variant ( pronounced m'yoo) in Colombia in January 2021. Since also, countries in South America and Europe have reported outbreaks of Mu.
In the U.S., the CDC says Mu reached a peak in June 2021, when it made up lower than 5 of variants going around the country. As of early September, it had been steadily declining.
Still, scientists continue to track Mu. The World Health Organization (WHO) says this variant has mutations that might make COVID-19 vaccines and our vulnerable systems less effective against it. Beforehand data suggests it has certain parallels to the Beta variant, but we need further exploration to know for sure.
In August 2021, the WHO labeled Mu a “ variant of interest.” In general, variants of interest might pose an arising threat to the world's public health, with the eventuality to do effects like spread more fluently, beget worse complaint, or shirk vaccines or tests. But they are considered lower of a trouble than “ variants of concern,” like Alpha, Beta, Gamma, and Delta.
As of September 2021, the CDC had not escalated Mu to being a variant of interest in the U.S. The agency intends to keep tracking it along with the other variants.
R. 1. Scientists first detected R. 1 in a number of countries, including Japan. There was an outbreak at a Kentucky nursing home in March 2021, when an unvaccinated health care worker passed it to about 45 other staff and presiders.
The WHO labeled it a “ variant under monitoring” in April 2021, meaning some of its characteristics may pose a unborn threat to humans.
As of October 2021, the CDC had not labeled R. 1 as a variant of concern or interest.
Epsilon, Theta, and Zeta were at one point listed as variants of interest and were downgraded by the WHO. They're still being covered.
Before Coronavirus Variants
Before in 2020, when the epidemic was new, you might have heard that there was further than one strain of the new coronavirus. Is it true? The answer appeared to be yes.
The proposition about different variants of the new coronavirus came from a study in China. Experimenters were studying changes in coronavirus RNA over time to figure out how colorful coronaviruses are related to each other. They looked at 103 samples of the new coronavirus collected from people, and they looked at coronaviruses from creatures. It turned out that the coronaviruses plant in humans were not all the same.
There were two types, which the experimenters called “ L” and “S.” They are veritably analogous, with slight differences in two places. It looks like the S type came first. But the scientists say the L type was more common early in the outbreak.
learn more about Coronavirus (COVID-19) Vaccines



